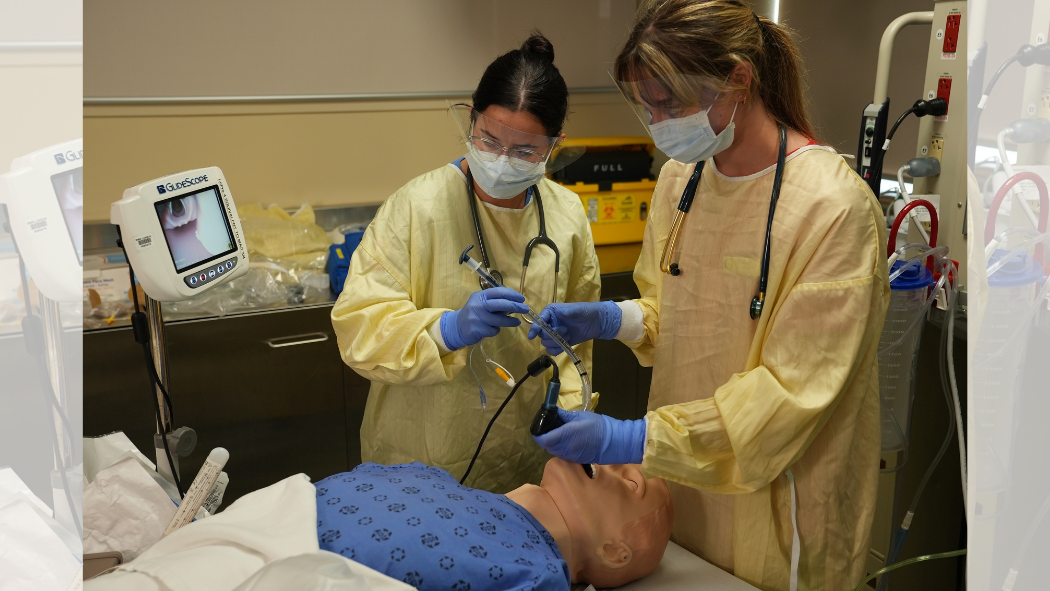
Image: From left to right, Charlize Barrow and Bailey Narasnek, RT students, simulating the intubation process on a simulation manikin.
October 26, 2023
A respiratory therapist (RT) is a crucial member of care teams for a variety of patient populations across London Health Sciences Centre (LHSC).
One of the ways RTs help support patient care is through providing intubation when needed on critically ill patients or patients undergoing surgery.
Intubation allows RTs to take over the breathing function for a patient for a variety of reasons. The video below has Samantha DaCosta, Charge Registered Respiratory Therapist, at University Hospital, narrating the steps taken to intubate a patient while two RT students, Charlize Barrow and Bailey Narasnek, demonstrate.
Intubation process
When a patient has been sedated and equipment made ready, the RTs will:
- Take the “blade”, and gently guide the curved device down a patient’s throat to visualize the vocal cords and the entrance into the trachea / lungs.
- Watch the procedure on the Glidescope to make sure the blade does not damage teeth or other internal structures in the patient’s trachea.
- Put the endotracheal tube down the middle of the “blade” structure and remove the rigid stylet in the blade so the tube can slide down the rest of the way. The rigid stylet helps keep the shape of the endotracheal tube so it can be more easily guided down a patient’s throat.
- Inflate the balloon and attach manual resuscitator to end of endotracheal tube.
- Begin breathing for patient.
- Once manual breathing begins, RTs:
- Ensure the endotracheal tube is in the correct location by listening to the patient’s chest with a stethoscope.
- Check for carbon dioxide coming through the endotracheal tube when patients breathe out to ensure that the tube is in the lungs.
- Check chest to make sure they hear air entry for both right and left lungs.
- Place device on patient’s face that holds endotracheal tube in correct placement and does not slip out.
Reasons for an intubation
A person may need intubation for a variety of reasons including for sleep during surgery, if a person has ALS and is unable to breathe on their own, or if a person is critically ill and they need to be placed in a medically induced coma while their care team helps treat their condition.
Areas where intubation is used
Respiratory therapists are largely seen in the intensive care units, operating room (OR) or the emergency department (ED) to support patients with cardio-respiratory concerns.
Respiratory therapists remain as calm and controlled as possible as they respond to patients in emergent situations such as a heart attack or a patient coughing up blood.
When intubating a patient in the OR, the situation is often more controlled with more stable and prepared patients. For example, they likely have not eaten prior to surgery, to ensure their stomachs are empty and have less risk for vomiting.
However, when a patient is in an emergent condition, their vital signs and conditions are more unstable and they may have recently eaten. Because of these reasons, there is a risk that food may come back up and potentially enter the lungs during the intubation procedure. This is called “aspiration.”
When a patient aspirates, there is a high risk of infection. Because of this, respiratory therapists use a specialized process called a rapid sequence induction (RSI) to help prevent aspiration in these situations. With an RSI, respiratory therapists use fast acting medications and a quick, deliberate intubation technique to protect the lungs and airway in cases where vomiting may be a concern.
Intubation is one of the ways that respiratory therapists, as part of interdisciplinary teams, provide person-centred care to patients across LHSC.
View the "What is intubation? How Respiratory Therapists intubate a patient" video PDF transcript.
