Framework
This section presents the LHSC framework for the delivery of care and services to LTV population. Although the goals of this framework are specific to individuals within the LHSC, it is recognized that many of these highly specialized resources are actually provincial resources, and must continue to be available beyond LHSC. A Long-Term Ventilator Strategy is in place to ensure that individuals across the province continue to have access to the needed services. The goals of this framework is to:
- To improve the overall experience of care and support for ventilator-assisted individuals and those at risk of long-term ventilation.
- To help ventilator-assisted individuals remain in the community longer, with an improved quality of life.
- To ensure timelier and more appropriate patient flow and transitions and enhance quality of care.
- To reduce avoidable emergency department visits and unnecessary acute care admissions
- To reduce alternate level of care (ALC) days
- To improve the patient experience
London Health Sciences Centre helps to care for many persons requiring chronic mechanical ventilation within the West Hub. These are individuals who enter our hospital system from a variety of access sites. This may occur through:
A) Our critical care units ,
B) ‘At Risk’ Outpatient clinics, or
C)Transition from Paediatrics.
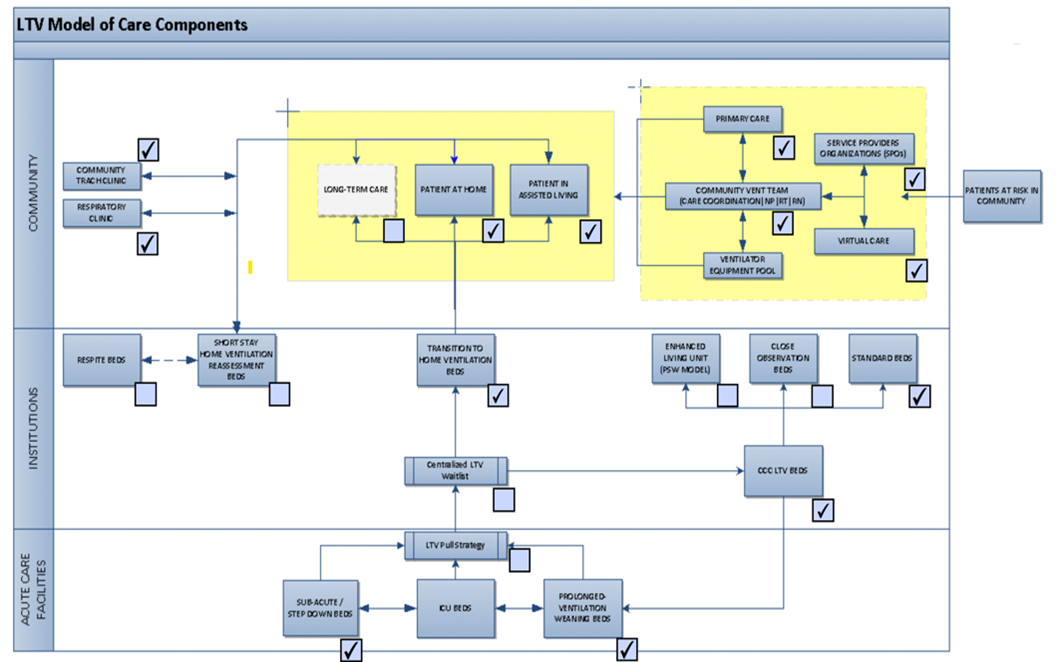
This service delivery model recognizes that ventilator-assisted individuals move back and forth along the continuum of care, experiencing encounters with a multitude of service providers (public and private, acute and complex continuing care, institutional and community) over the course of their lives. Ensuring individuals are in the right setting, or are transferred to the right setting in a timely manner, requires an integrated service delivery model with collaboration and cooperation of service providers across the full continuum of care to address all of the LTV population’s needs. Consistent with the West Hub’s population-based integration model, the above service delivery model focuses on providing the infrastructure and communication tools needed to support this population, managed through intensive case management, where necessary, and supported by access to an electronic health record for each member of this population.
The flow map was developed for three scenarios:
- Ventilator-assisted individual in an ICU, at risk of prolonged mechanical ventilation.
- Ventilator-assisted individual in a CCC unit.
- At-risk or ventilator-assisted individual living in the community
Note that for the purpose of these flow maps, the term community is defined as a private home, supportive housing, or long-term care home.
This map is intended to cover the majority of settings and circumstances for the target population. Note that the flow map is based on the assumption that the at-risk or ventilator-assisted individual is already in the most appropriate setting and also that it is drawn to illustrate the movement of an individual through the continuum of care and services from the perspective of the at-risk or ventilator-assisted individual.
Although individuals may have different reasons for requiring mechanical ventilation e.g., different types of respiratory and neuromuscular disease, they all have chronic alveolar hypoventilation. Central to our system of care has been the establishment of a interdisciplinary outpatient process designed to regularly follow individuals requiring chronic ventilator care (either invasive or non-invasive)and those ‘at risk’ of developing respiratory failure. Dedicated resources, both technological and human, are needed to provide these individuals access to specialized respiratory (and related) care needs, as close to home as possible, or ideally at home.



